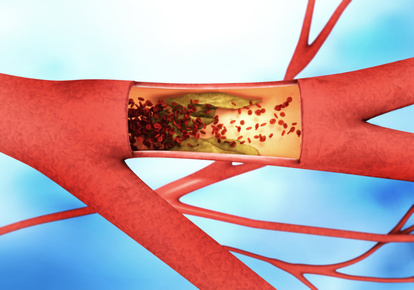
In mice, Professor Oliver Söhnlein from the LMU Hospital Munich and his team mimicked an acute bacterial infection to understand the increased risk of heart attack better. The mice also had atherosclerosis and were, therefore, a suitable model for cardiovascular patients at risk of infarction. In atherosclerosis, the blood vessels' inner wall is chronically inflamed, and deposits called plaques form. When these deposits break loose, they can trigger a heart attack or stroke. The researchers observed that the infection increased the size of the mice's plaques and boosted inflammation.
Positively charged attractant
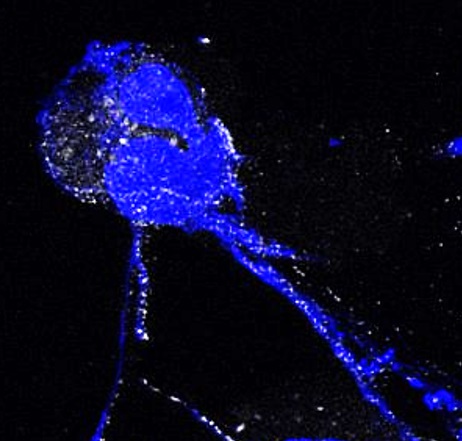
A closer look at the vascular plaques showed that certain immune cells, the neutrophils, accumulated there. The infection had activated them, causing them to release so-called NETs (Neutrophil Extracellular Traps). NETs consist of DNA and proteins that originate from inside the neutrophils and actually serve to bind pathogens. The Munich researchers found that in NETs, the protein histone H2a also attracts other immune cells, the monocytes. "Histone H2a is strongly positively charged and is normally present in the cell nucleus," Söhnlein explains. "With the release of NETs, it gets to the outside. The cell surface of monocytes is negatively charged, so they stick to the positively charged histone H2a and thus to the debris." The monocytes then penetrate the vessel wall, where they turn into macrophages. In this way, they cause inflammation and promote the formation of dangerous deposits.
Mini proteins could protect against heart attacks
When the scientists used antibodies against histone H2a or very small, specific proteins that only bind to histone H2a, less monocytes adhered to histone H2a, and acceleration of atherosclerosis was slowed down.
This opens up a new therapeutic option for cardiovascular risk patients with an acute infection. Because small proteins, so-called peptides, directed against histone H2a could also prevent atherosclerotic lesions and the risk of heart attack from increasing in patients. Söhnlein and his collaborators have already filed a patent for these peptides.
Mitigating complications of COVID-19
"Viruses and other bacteria also trigger the release of NETs. If they also cause cardiovascular complications, infected patients could benefit from a therapy directed against NETs or histones. However, this would still have to be proven in follow-up studies," says Söhnlein. The Munich researcher is also thinking about SARS-CoV2. It has been known since spring last year that neutrophils are significantly involved in severe COVID-19 complications such as lung damage and thrombosis. There, too, these immune cells release NETs. The histones in the NETs activate blood clotting and thus trigger thrombosies. According to Söhnlein, a therapy targeting histones could, therefore, attenuate severe COVID-19 courses.
Original publication: Endotoxinemia Accelerates Atherosclerosis via Electrostatic Charge-Mediated Monocyte Adhesion. Schumski A, Ortega-Gómez A, Wichapong K, Winter C, Lemnitzer P, Viola JR, Pinilla-Vera M, Folco E, Solis-Mezarino V, Völker-Albert M, Maas SL, Pan C, Perez Olivares L, Winter J, Hackeng T, Karlsson MCI, Zeller T, Imhof A, Baron RM, Nicolaes GAF, Libby P, Maegdefessel L, Kamp F, Benoit M, Döring Y, Soehnlein O. Circulation. 2020 Nov 10.
DOI: 10.1161/CIRCULATIONAHA.120.046677
Scientific contact: Prof. Oliver Söhnlein, Institute for Prophylaxis and Epidemiology of Circulatory Diseases (IPEK), Polyclinic, LMU Hospital Munich, Ludwig-Maximilians-Universität Munich; Karolinska Institute, Stockholm, Sweden, Oliver.Soehnlein(at)med.uni-muenchen.de
Contact: Christine Vollgraf, Press and Public Relations, German Center for Cardiovascular Research (DZHK), Tel: 030 3465 529 02, presse(at)dzhk.de
Reduce heart attack risk after infections